Conditions & Treatments
Learn more about the conditions we treat at Spectrum Retina & Ocular Oncology
Adult and Pediatric Retinal Detachment
Retinal detachment occurs when the thin layer of tissue (the retina) at the back of the eye pulls away from the tissue around it. Most people notice flashes or floaters in their vision when this happens. Your retina can't work properly when this happens, and if not treated immediately, you could have permanent vision loss.
There are many causes of retinal detachment, but the most common causes are aging or eye injury. There are 3 types of retinal detachment: rhegmatogenous, tractional, and exudative.
1. Rhegmatogenous Retinal Detachment (RRD):
This is the most common form and can occur in children. A tear in the retina allows vitreous humor to further separate the two layers.
2. Tractional Retinal Detachment (TRD):
The retina is pulled away by abnormal tissue (fibrosis seen in diabetic retinopathy or retinopathy of prematurity). This commonly occurs in diabetic people due to the damaged blood vessels in the back of your eye.
3. Exudative Retinal Detachment (ERD):
Underlying barrier dysfunction leads to a collection of fluid building up behind your retina. This pushes your retina away from the tissue.
Examples: Vascular disease, Intraocular tumors.
The number of retinal detachments in children is rare, compared to the number of retinal detachments in adults; only 3-7% occur in children. The main predisposing factors are trauma, myopia, hereditary vitreoretinopathies, retinopathy of prematurity, malformations, and Coasts’ disease. The most frequent pediatric retinal detachments are trauma-associated and when the retina detaches, fluid accumulates in the potential space created by this tear. The more the retina is involved, the macula may become involved and threaten vision. While retina detachment is less common in children, the median age is 9 to 13 years.
An eye exam can also identify early changes that may go unnoticed. Get your eyes checked once a year, or more often if you have conditions like diabetes or very nearsighted.
Give us a call at 703-643-9328 today to schedule a consultation.
Choroidal Melanoma, hemangioma, and other tumors of the choroid
There are several tumors of the Choroid, which affect both adults and children alike.
Choroidal Melanoma affects the 3 main layers of the wall of the eye. Starting at the outside, there is the white sclera, a blood vessel layer called the urea (choroid, Hillary body, and iris), and an inner retinal layer. Melanocytes are the pigment producing cells and are primarily found in the vascular uveal layer. The melanocytes can turn into malignant melanoma. When melanoma happens in the chord, they are called “choroidal melanoma”. This is the most common malignancy in adults. Choroidal melanomas are rare, in that 5 to 10 out of a million people are diagnosed with a choroidal melanoma each year. This melanoma can spread to other parts of the body. An ultrasound can evaluate and detect choroidal melanoma associated retinal detachment.
Choroidal Hemangioma is a benign vascular hamartoma that occurs most of the time in a solitary form but may also present as a diffuse form. It is unclear what causes a choroidal hemangioma. Cavernous hemangioma of the retina are usually non-progressive, and observation is the best management. No treatment has been shown effective or necessary.
Choroidal nevi are common and occur in about 5-10% of the population. A choroidal nevus is a flat, benign pigmented area that appears in the back of the eye. This develops in the vascular layer under the retina.
A nevus is caused by the growth of cells called melanocytes. These cells produce the colors of your skin, hair, and eyes. When the cells clump together, they can form this darker spot called a nevus. These pigmented areas need to be monitored to ensure they don’t cause problems but normally remain benign.
Retinoblastoma
Retinoblastoma is an eye cancer that begins in the back of your eye at the retina. This occurs most commonly in children (often under 5 years of age), affecting the retina of your eye. If a pupil appears white when light is shined into the eye, sometimes with flash photography or eyes may appear to be looking in different directions, this can indicate cancer.
When diagnosed early, this eye cancer is often curable through chemotherapy, radiation, or laser therapy. Retinoblastoma has one of the best cure rates of all childhood cancers (95-98%), with more than 90% of sufferers surviving into adulthood.
A typical retinoblastoma is a round or oval-shaped, variably vascularized pink mass. It may sometimes appear chalky white, because of calcification. Retinoblastoma is composed of small, round densely packed cells with large hyperchromic nuclei.
Endophytic retinoblastoma grows into the vitreous cavity and accounts for 60% of typical retinoblastomas. Retinoblastoma accounts for 4% of all pediatric cancers and the percentage overall is 1 in 18,000 to 30,000 live births per year, regardless of sex, race, or geographic predilection. Each year, 5,000 to 8,000 new cases of retinoblastoma are diagnosed on a global scale. Retinoblastoma is responsible for 1% of all deaths below 15 years of age.
For treatment, systemic chemotherapy has become the most commonly used method worldwide within the past 10 years for almost all intraocular retinoblastoma. Local chemotherapy is used to deliver higher concentrations into the eye and avoid systemic toxicity and side effects. Enucleation is a surgical treatment that is indicated for most cases where there is no prospect of vision. Cryotherapy is a method of rapid freezing of the tumor.
Vitreoretinopathies:
FEVR, X-linked Retinoschisis, Stickler Syndrome, PFVS, etc.
Familial exudative vitreoretinopathy (FEVR) is a hereditary disorder that can cause progressive vision loss. This condition affects the retina, the specialized light-sensitive tissue that lines the back of the eye, which prevents blood vessels from forming at the edges of the retina and reduces the blood supply to the tissue. The signs and symptoms vary widely within the same family. Many people never have any vision problems, while others have a reduction in the retina's blood supply, causing the retina to fold, tear or separate from the back of the eye (retinal detachment). This damage can lead to vision loss and blindness. Some people with this disorder also have reduced bone mineral density, which weakens bones and increases the risk of fractures. Sometimes, the cause of familial exudative vitreoretinopathy is unknown.
X-linked Juvenile Retinoschisis is a disorder that begins in childhood and occurs almost exclusively in males, affecting the retina. Damage that is done to the retina impairs the sharpness of vision in both eyes and typically, x-linked juvenile retinoschisis affects the cells in the central area of the retina called the macula, which is responsible for the sharp central vision that is needed for detailed tasks, such as reading, driving and recognizing faces. This is a type of broader disorder called macular degeneration, which disrupts the normal function of the macula and sometimes affects the side (peripheral) vision. This disorder is usually diagnosed when affected boys start school. By the time a man is in his fifties or sixties, sometimes severe complications develop, such as separation of the retinal layers (retinal detachment), or leakage of blood vessels in the retina (vitreous hemorrhage, which can further impair vision or cause blindness).
Stickler syndrome is a group of hereditary conditions, characterized by a distinctive facial appearance, eye abnormalities, hearing loss, and joint problems. Stickler syndrome or severe nearsightedness is a disorder in which the clear gel that fills the eyeball (the vitreous) has an abnormal appearance, and is noticeable during an eye examination. Stickler syndrome affects an estimated 1 in 7,500 to 9,000 newborns.
Persistent Fetal Vasculature (PFV) disorder occurs when the vascular structures present during the development of the eye fail to wither or regress as they should. The resulting structural abnormalities may lead to impairment of vision. The disease itself is usually not progressive, but as the eye grows, the abnormal structural components of PFVS do not grow along with it; traction from the abnormal tissues on structures within the eye increases, and progressive changes may occur. This disorder often becomes apparent at birth or shortly thereafter.
Crossed eyes (strabismus), abnormal eye movements (nystagmus), and lazy eye (amblyopia) are common symptoms. Often, eyes with PFV are smaller than normal and sometimes only one eye is affected. However, there are instances in which the eyes are normal in size, or where both eyes are smaller than normal. The most important disease to rule out when a child shows signs of leukocoria is retinoblastoma (a rare malignant tumor of the retina). Most commonly, the lens is removed, and on occasion, surgery is also done to reattach the retina.
Diabetic Retinopathy and retinal complications of systemic diseases and treatments
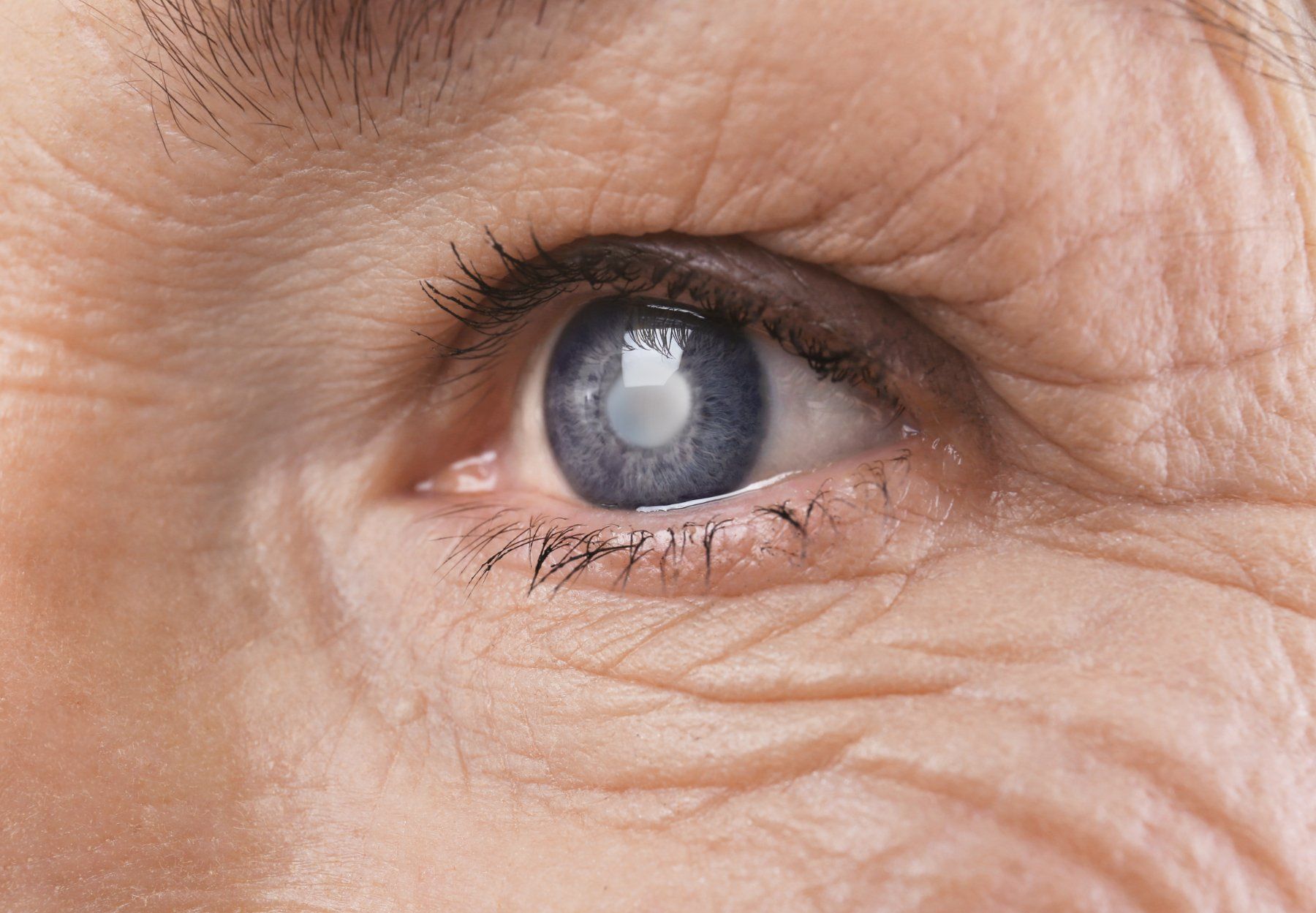
Diabetic retinopathy is a diabetes complication that affects the eyes. It's caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). While the beginning of the complication may lack symptoms or only cause mild vision problems, eventually this disease can cause blindness.
This condition can develop in anyone who has type 1 or type 2 diabetes. People who have diabetes for longer periods and don’t regulate their blood sugar are more likely to develop this complication. Diabetic retinopathy generally affects both eyes which may include these symptoms:
— Spots or dark strings floating in your vision (floaters)
— Blurred vision
— Fluctuating vision
— Impaired color vision
— Dark or empty areas in your vision
— Vision loss
There are two types of diabetic retinopathy:
1. Early Diabetic Retinopathy:
This form is more common, called nonproliferative diabetic retinopathy (NPDR). New blood vessels aren’t growing and the walls of the blood vessels in your retina weaken.
Tiny bulges (microaneurysms) stick out from the smaller vessels, potentially leaking fluid and blood into the retina. This causes larger vessels to dilate and become irregular. Nerve fibers may begin to swell, along with the central part of the retina (macula) which requires treatment.
2. Advanced Diabetic Retinopathy:
This type is more severe, progressing from the early stages. Damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina, and can leak into the clear, substance that fills the center of your eye (vitreous).
The growth of new blood vessels may cause scar tissue to develop, which might detach your retina from the back of your eye. Pressure may build if the new blood vessels prevent the normal flow of the fluid in your eye. This can damage the nerve that carries images to your brain, resulting in glaucoma.
Retinal Vascular Diseases
Retinal Vascular Disease is a disorder of the retina and the eyes depend on the flow of oxygen rich blood to function.
The eyes have nerves and tissues which send signals to the brain to create a visual image. The retina is one of the tissues and is located at the back of the eye. The retina plays a crucial role in sending signals to the brain and contains small and large arteries and veins that move blood to and from the heart. Since blood is essential to vision, a blockage in the retina's blood vessels can permanently affect vision and lead to blindness.
An eye stroke is also known as retinal artery occlusion and is caused by a clot or narrowing of the retina's blood vessels, and the blood flow is interrupted. If left untreated, the result can be permanent damage to the retina and loss of light. Much like a cerebral stroke, the brain is reduced or cut off, and the retinas in the eye lose their blood supply. The risk is similar to that of a regular stroke. Some people have floaters or blind spots and may also have distorted vision.
Retinal Occlusion (RVO) is a common vascular disorder of the retina and one of the most common causes of vision loss worldwide and the second most common cause of blindness.
Macular Pucker and Macular Hole
The macula (central part of the retina) is essential for high-definition vision. Conditions that damage or distort the macula can result in blurred or distorted vision. Two common conditions that affect the macula are macular puckers and macular holes.
A macular pucker is a thin layer of scar tissue that forms on top of the retina. These can range from mild to severe, with some hardly noticeable during an exam while others cause a wrinkle of the macula. People with a macular pucker might notice mild blurring in their central vision, or for the more severe puckers, straight items appear to have a bend in the structure.
The macular hole is more severe and is a small gap that extends through the entire thickness of the macula. Small holes may only distort or blur your vision, while larger ones result in a central blind spot.
The most common cause of these conditions is aging. However, certain diseases like diabetes that affect the retinal blood vessels can also cause macular conditions.
Ocular Oncology
Ocular oncology involves the diagnosis and treatment of all tumors that occur in or around the eye - tumors of the eye, eyelid, orbit and tear, or lacrimal glands. Ocular tumors affect adults and children, and tumors may occur in one eye or may involve both eyes.
Ocular tumors can range from harmless to potentially life-threatening. They may also cause vision loss or loss of the eye itself depending on the severity.
— Eye cancer survival rates depend on the type of tumor along with its size and location.
— The 5-year survival rate for people with eye cancer is 80-85%.
— 73% of people are diagnosed at an early stage.